Our genetics, life history, and lifestyle all influence when and how we experience the Peri-2-Post Transition. However, there are some general patterns that women go through if this transition occurs naturally (not medically induced). And, just as our experiences are unique, the solutions that work best for each of us are also unique.
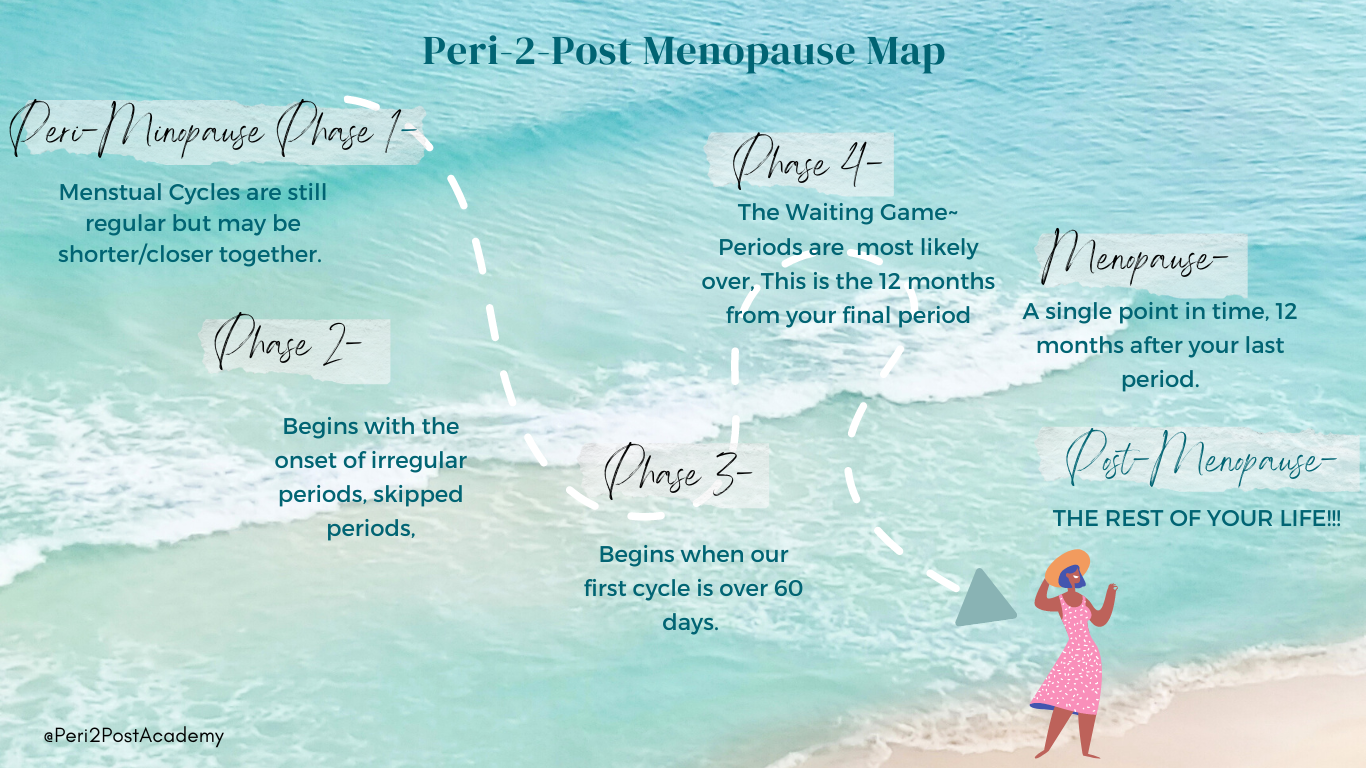
Typically, Perimenopause transition is divided into two stages: the early stage and the late stage. Hormone levels fluctuate during the early stage, and estrogen production decreases during the late stage. Looking at it from a biochemical/hormonal perspective, I see there is a clear breakdown of Perimenopause into 4 Phases. Each phase is linked to specific symptoms that may arise due to these biochemical changes. Let’s delve deeper into this transition…
Peri-2-Post Phase 1
The initial phase of perimenopause is defined by lower progesterone levels.
Menstrual periods are generally still regular in terms of timing throughout the initial phase of perimenopause. However, during this stage, ovulation is not as robust and thus the cells that make your progesterone are not as productive. You may also have a reduction in the frequency of ovulation. Both lead to an overall lower progesterone level. This can influence your menstrual cycle. The length between cycles may change by a day or two, the duration, and flow of blood can change, there may be mid-cycle spotting and PMS symptoms may worsen. A decrease in progesterone levels is the root cause of these changes. Although your estrogen levels may remain relatively constant, the balance between estrogen and progesterone is disrupted.


Peri-2-Post Phase 2
During the second stage, our cycles become more irregular and may vary in length by more than 6 or 7 days. During this stage, you may have low progesterone levels and estrogen levels that are often higher but vary.
During this stage, women may oscillate between anovulatory (decreased estrogen, an egg is not released) and normal cycling. An anovulatory cycle leads to an increase in early high FSH levels in the following cycle. This increased FSH level leads to the development of a greater number of ovarian follicles developing, each producing more estrogen, resulting in significantly higher estrogen levels than usual.
This indicates that while the overall estrogen levels remain elevated, the fluctuations are becoming more noticeable, particularly with distinct low points. With estrogen levels starting at a higher point, they not only have more room to decrease but can also drop lower than usual.
This leads to symptoms of low estrogen such as headaches, depression, weight gain, vaginal dryness, and night sweats, and symptoms of excess estrogen like allergy symptoms, irritability, anger, fluid retention, and breast soreness.
Peri-2-Post Phase 3
It is during this stage that we begin to experience irregular periods and our first cycle that lasts for more than 60 days.
The symptoms of elevated estrogen may begin to subside because of lower estrogen, even though it may still fluctuate during Stage 3 of the Peri-2-Post transition.
Menstrual cycles become exceedingly irregular, and they are becoming more infrequent. Circulating estrogen is more likely to be low during anovulatory cycles, and the prevalence of low estrogen symptoms increases significantly during extended periods without a cycle. An occasional burst of elevated estrogen may be observed, but the overall pattern is low progesterone and estrogen.
As an outcome, symptoms associated with elevated estrogen levels may diminish, while those associated with low estrogen levels often worsen.


Peri-2-Post Phase 4
This is the phase when our menstrual cycles are much less frequent to most likely finished and we have ceased ovulating. However, since a full year has not yet passed, we have not formally entered menopause.
It is the consistently low levels of estrogen that results in a reduction of symptoms associated with high and variable estrogen. As a result, headaches and migraines may be becoming more stable.
It is important to note that hot flashes may persist for some time.
The prevalence of depressed mood and heightened anxiety tends to grow abruptly when women approach the later stages of the menopausal transition and experience prolonged periods without menstruation. These symptoms frequently interact, resulting in depressed women experiencing more severe hot flashes, night sweats and sleep disturbances.