Stage 3 Perimenopause: When Estrogen Truly Declines
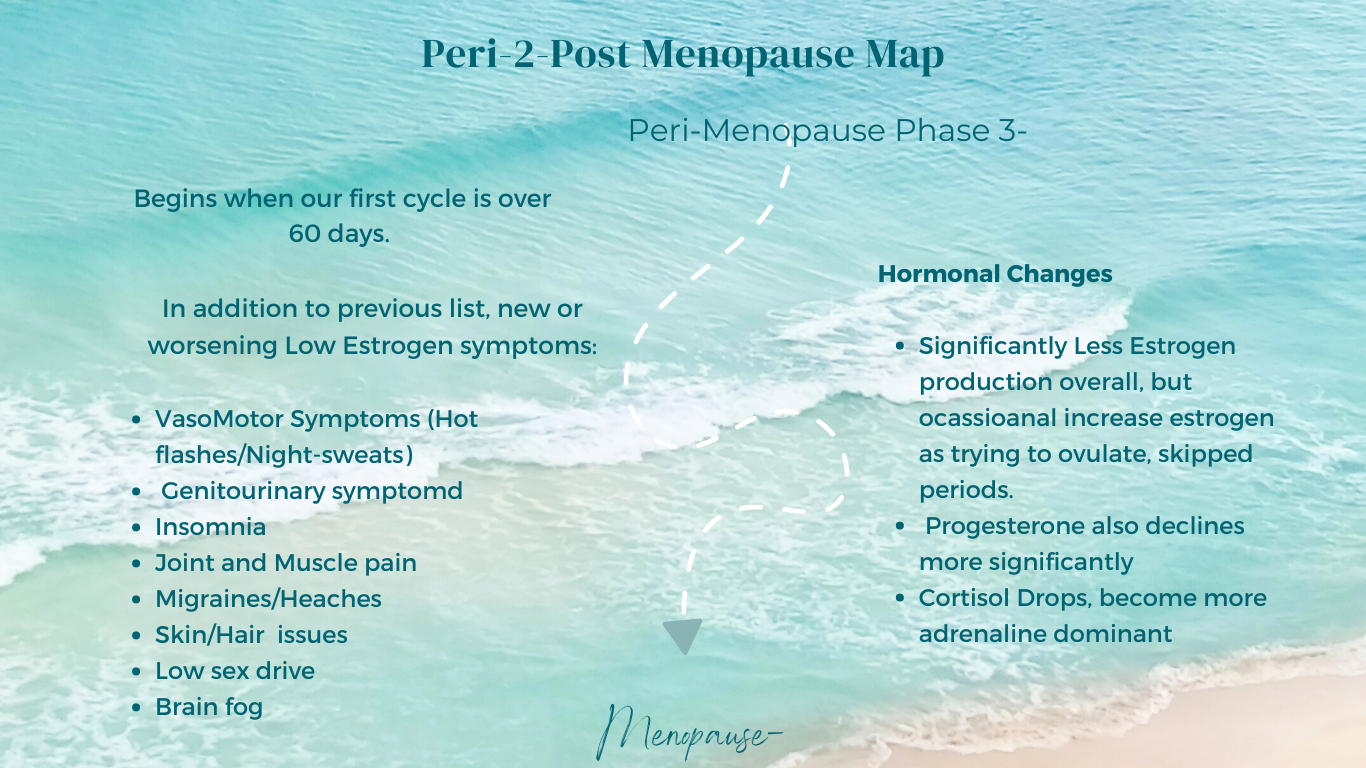
Stage 3 perimenopause begins when cycles become widely irregular — including your first cycle longer than 60 days.
This stage marks a shift from hormonal volatility to overall hormonal decline.
While estrogen may still fluctuate occasionally, the dominant pattern becomes:
Low progesterone
Low estrogen
Irregular or absent ovulation
Symptoms begin to reflect sustained estrogen withdrawal rather than dramatic swings.
What Is Happening in Stage 3 Perimenopause?
During earlier stages, estrogen fluctuates sharply. In Stage 3, circulating estrogen is more consistently low, especially during extended stretches without ovulation.
You may still experience occasional bursts of higher estrogen, but the overall pattern trends downward.
As estrogen declines, symptoms associated with high estrogen often subside.
Low-estrogen symptoms become more prominent.
Common Symptoms of Stage 3 Perimenopause
• Hot flashes and night sweats
• Vaginal dryness
• Low libido
• Brain fog
• Insomnia
• Migraines
• Joint and muscle pain
• Thinning skin
• Hair thinning or loss
• Tinnitus or ear itching
These symptoms reflect estrogen’s systemic role.
Estrogen is not just a reproductive hormone.
It influences the brain, skin, connective tissue, vascular system, immune function, and nervous system.
The Biochemistry Behind Stage 3 Symptoms
Vasomotor Symptoms (Hot Flashes & Night Sweats)
Estrogen stabilizes the hypothalamus, the brain’s temperature regulation center.
As estrogen declines:
• Thermoregulatory neurons become hypersensitive
• Small temperature shifts trigger exaggerated cooling responses
• Blood vessels dilate
• Sweating increases
• Heart rate rises
This is why hot flashes can feel sudden and intense.
Triggers may include alcohol, stress, altitude, and spicy foods.
Migraines and Headaches
Women experience migraines at significantly higher rates than men, particularly during puberty and perimenopause.
Research suggests estrogen withdrawal plays a key role in migraine pathophysiology.
As estrogen levels fall:
• Neurovascular regulation shifts
• Inflammatory pathways activate
• Serotonin signaling changes
However, migraines are multifactorial. Histamine, food sensitivities, stress, and sleep disruption may also contribute.
Common triggers include:
• Alcohol
• Aged cheeses
• Gluten
• Food additives
• High-histamine foods
Magnesium-rich foods, anti-inflammatory nutrition, and consistent sleep patterns may help reduce frequency.
Skin Changes and Collagen Loss
Estrogen supports collagen production through estrogen receptors located on fibroblasts.
When estrogen declines:
• Collagen synthesis decreases
• Skin becomes thinner
• Elasticity reduces
• Hydration declines
• Wrinkling accelerates
Women may lose up to 30% of facial collagen within the first five years of menopause.
Estrogen also supports:
• Hyaluronic acid production
• Elastin formation
• Wound healing
• Vascularization
• Protection from oxidative stress
Supporting Skin Health
• Hydration
• Antioxidant-rich nutrition
• Topical vitamin C and E
• Retinol
• Moisturizers containing hyaluronic acid or ceramides
• Red light therapy
• Collagen supplementation (hydrolyzed collagen may improve elasticity)
Topical estradiol, estriol, or DHEA may be considered under medical supervision.
Hair Thinning and Loss
Hair follicles cycle through growth (anagen), transition (catagen), and rest (telogen).
Estrogen and progesterone help maintain hair in the growth phase.
As these hormones decline:
• Hair growth slows
• The resting phase lengthens
• Androgen effects become more prominent
• Follicles miniaturize
Reduced scalp blood flow due to decreased vasodilation may also contribute.
Additional contributors include:
• Thyroid dysfunction
• Cortisol dysregulation
• Nutrient deficiencies
• Metabolic shifts
Nutrients such as biotin, zinc, iron, vitamin D, and adequate protein intake support hair health.
Tinnitus and Ear Sensitivity
Estrogen receptors are present in auditory pathways and cochlear hair cells.
Declining estrogen may:
• Alter blood flow to the inner ear
• Influence electrical signaling
• Increase sensitivity to auditory stimuli
Some women experience itching, fullness, or ringing in the ears during this stage.
The precise hormonal mechanisms are still under investigation.
Supporting Stage 3 Perimenopause
At this stage, the goal shifts from managing volatility to supporting systemic resilience.
Strategies include:
• Strength training to preserve muscle and bone
• Anti-inflammatory nutrition
• Stress regulation
• Cardiovascular support
• Sleep hygiene
• Evaluation for hormone therapy when appropriate
Individual factors, genetics, life history, metabolic health, shape how this stage unfolds.
There is no universal protocol.
Frequently Asked Questions About Stage 3 Perimenopause
When does Stage 3 perimenopause begin?
It typically begins when cycles extend beyond 60 days and become markedly irregular.
Why do hot flashes worsen before menopause?
Sustained estrogen decline increases hypothalamic sensitivity.
Does low estrogen cause hair loss?
Estrogen supports hair growth and vascular supply to follicles. Decline may contribute to thinning.
Can perimenopause cause tinnitus?
Emerging research suggests estrogen influences auditory pathways, and hormonal decline may contribute to symptoms.
The Bigger Picture
Stage 3 perimenopause represents sustained hormonal decline rather than dramatic fluctuation.
Symptoms may feel more persistent, but they are not random.
They reflect estrogen’s systemic role.
Understanding the physiology allows you to respond strategically, not reactively.
Midlife is not a breakdown.
It is a transition requiring new information.