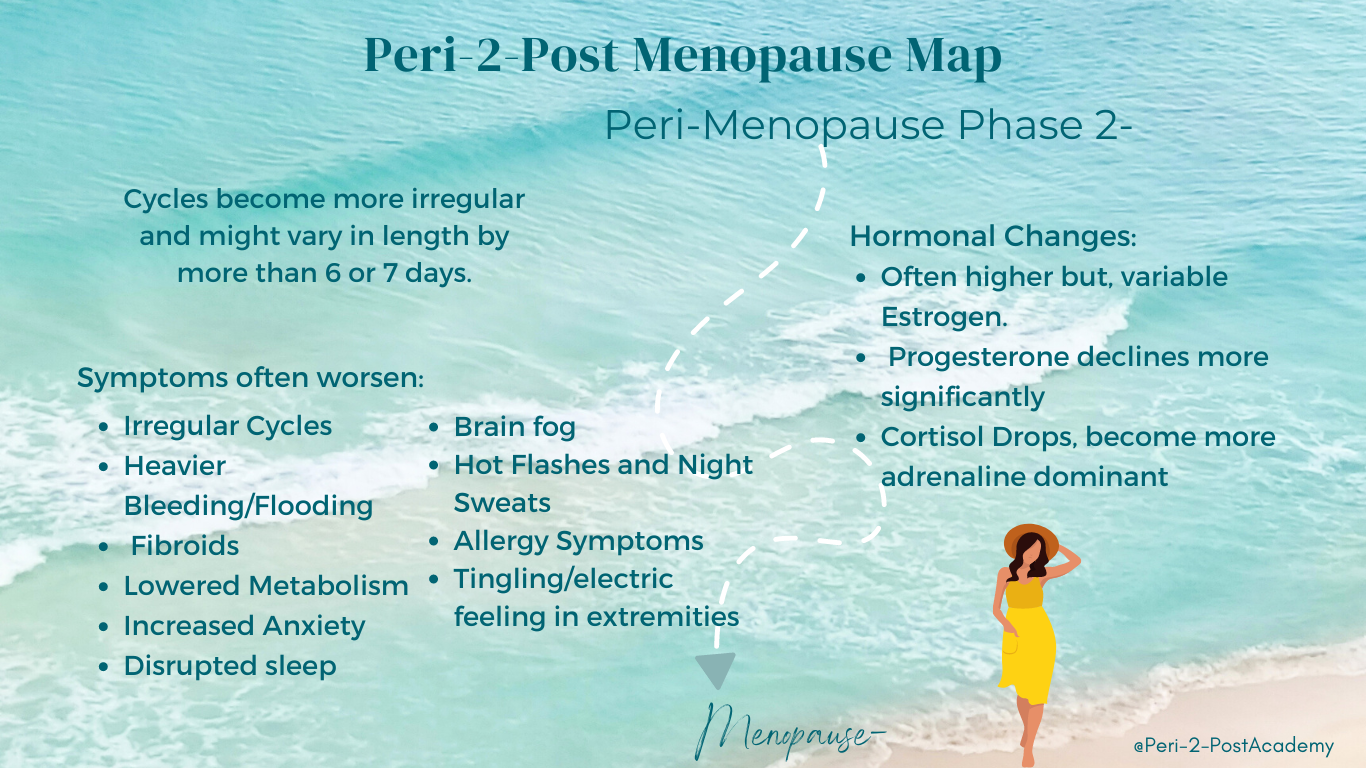
The second stage of perimenopause is defined by cycle irregularity and pronounced estrogen fluctuation.
During this phase, menstrual cycles may vary by more than 6–7 days in length. Ovulation becomes inconsistent, progesterone remains low, and estrogen levels may swing higher — and lower — than before.
This is not steady decline.
It is volatility.
And volatility creates symptoms.
What Is Happening in Stage 2 Perimenopause?
In this phase, women may alternate between:
• Anovulatory cycles (no ovulation, lower progesterone)
• Ovulatory cycles with elevated follicle stimulation
When ovulation does not occur, progesterone remains low.
The following cycle often begins with elevated FSH (follicle-stimulating hormone). Higher FSH stimulates the development of multiple ovarian follicles, each producing estrogen.
The result?
Higher-than-normal estrogen production — followed by dramatic drops.
Estrogen is not simply declining. It is fluctuating.
And fluctuation is physiologically disruptive.
Why Estrogen Fluctuations Feel So Intense
When estrogen rises higher than usual and then falls rapidly:
• The nervous system reacts
• Thermoregulation destabilizes
• Mood regulation shifts
• Histamine sensitivity increases
Because estrogen interacts with the brain, immune system, vascular system, and connective tissue, its instability affects multiple systems simultaneously.
This is why Stage 2 symptoms often feel widespread and unpredictable.
Common High Estrogen Symptoms in Stage 2
• Breast tenderness
• Heavy or painful periods
• Increased cervical mucus
• Fluid retention
• Histamine-related symptoms (allergy-like reactions)
• Irritability or agitation
• Sleep disruption
Common Estrogen Withdrawal (Low Estrogen) Symptoms
• Hot flashes
• Night sweats
• Vaginal dryness
• Headaches
• Mood changes
• Abdominal weight gain
• Joint aches
• Poor sleep
Women often experience both sets of symptoms within the same month.
That’s the hallmark of this stage: oscillation.
The Biochemistry Behind Key Symptoms
Vasomotor Symptoms (Hot Flashes & Night Sweats)
Fluctuating estrogen levels increase the sensitivity of neurons in the hypothalamus — the brain’s temperature regulation center.
When estrogen drops:
• The hypothalamic thermostat becomes overly sensitive
• Small increases in body temperature trigger exaggerated cooling responses
• Blood vessels dilate
• Sweat glands activate
• Heart rate increases
This is why hot flashes can feel sudden and intense — sometimes accompanied by palpitations.
Genetics, race, cardiovascular health, and vascular stiffness all influence severity.
Triggers may include:
• Alcohol
• Spicy food
• Altitude
• Acute stress
• Anxiety
Mood Swings, Anger, and Irritability
Estrogen influences:
• Serotonin production
• Serotonin receptor sensitivity
• Endorphin signaling
• Neural growth and protection
When estrogen levels fluctuate dramatically, mood regulation becomes less stable.
Women with a history of severe PMS or depression may experience more pronounced mood changes during this stage.
Tingling or Electric “Zaps”
Declining estrogen influences peripheral nerve signaling and circulation.
Low estrogen may:
• Increase nerve hypersensitivity
• Reduce peripheral blood flow
This can lead to:
• Tingling
• Pins-and-needles sensations
• Electric shock-like “zaps,” often preceding hot flashes
Important: Always rule out other medical causes such as diabetes, vitamin deficiencies, or nerve compression.
New or Worsening Allergy Symptoms
Stage 2 perimenopause often coincides with increased histamine sensitivity.
Estrogen stimulates histamine release.
Histamine can stimulate further estrogen activity.
This feedback loop may worsen:
• Anxiety
• Digestive issues
• Headaches
• Heavy bleeding
• Hives
• Runny nose
• Itchy skin
• Sleep disruption
Histamine symptoms often intensify during high-estrogen swings.
Frequently Asked Questions About Stage 2 Perimenopause
Why are my cycles suddenly irregular?
Ovulation becomes inconsistent, and estrogen production fluctuates significantly during this stage.
Why do I feel both high-estrogen and low-estrogen symptoms?
Because estrogen levels may swing dramatically within a single cycle.
Why do hot flashes start before menopause?
Fluctuating estrogen increases hypothalamic sensitivity well before estrogen fully declines.
Can allergies worsen during perimenopause?
Yes. Estrogen and histamine interact in ways that can intensify immune responses.
The Bigger Picture
Stage 2 perimenopause is not steady decline.
It is hormonal volatility.
Understanding the mechanism behind the symptoms restores perspective.
This transition is not random — and it is not personal failure.
It is adaptive physiology in motion.
When you understand the system, you can support it strategically.